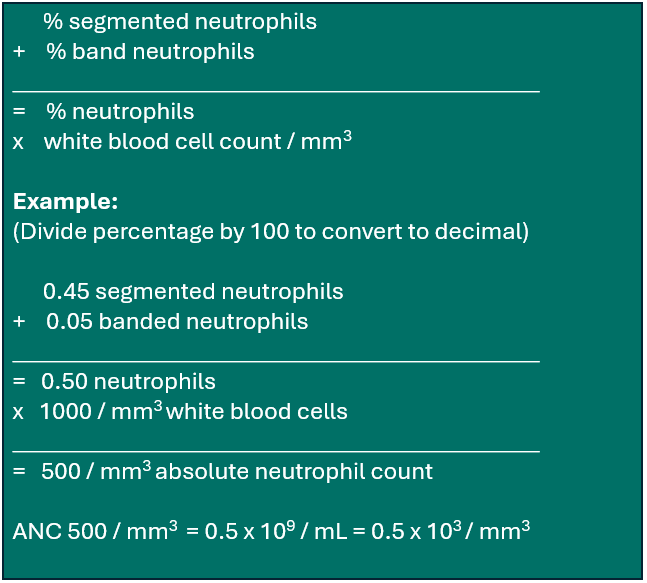
ANC recovery is defined as an absolute neutrophil count (ANC) of ≥ 0.5 × 109/L (500/mm3) for three consecutive laboratory values obtained on different days. Date of ANC recovery is the date of the first of three consecutive laboratory values where the ANC is ≥ 0.5 × 109/L. At some institutions, the laboratory reports display the ANC value once there are sufficient white blood cells to perform a differential count. At other institutions, the laboratory reports do not display the ANC, and it must be calculated from the white blood cell count (WBC) and the percent of segmented and band neutrophils (if the differential was performed on a machine, the percent neutrophils will include both segmented and band neutrophils). If the laboratory report displays an automated ANC value of exactly 0.5, the actual ANC value should be calculated from the manual differential if available. The calculated value from the manual differential will determine ANC recovery. If your institution’s laboratory reports do not display the ANC value, use the following calculation to determine the ANC:
Calculating Absolute Neutrophil Count (ANC)1
1 Traditionally, the definition of ANC recovery required selecting the first date of three consecutive days in which the recipient’s ANC was ≥ 0.5×109/L (500/mm3). For various reasons it may not be possible to obtain daily laboratory values. Under those circumstances, report ANC recovery based upon three consecutive laboratory values (drawn more than a day apart) as long as the ANC remains ≥ 0.5×109/L (500/mm3).
Tracking the date of ANC recovery may not always be straightforward. In some cases the ANC may fluctuate for a period of time before the recipient fully recovers. In other cases the ANC may remain above 0.5 × 109/L for several days immediately post-HCT and then fall below 0.5 ×109/L. Do not begin counting ANC values of ≥ 0.5 × 109/L towards recovery until the ANC has dropped to the lowest level (nadir) post-HCT. If the recipient was transplanted using a non-myeloablative (NST) or reduced intensity (RIC) regimen, or was transplanted for an immunodeficiency (e.g., SCID, WAS), the recipient’s ANC may never drop below 0.5 × 109/L. If this is the case, an ANC recovery date will not be reported, and the “never below” option should be chosen. However, if the recipient’s ANC drops below 0.5×109/L for even one day, this should be considered the nadir and “never below” should not be chosen. See the following example for more information regarding tracking the date of ANC recovery.
Tracking ANC Recovery
Transplant Date = May 6| Date | WBC | %Neutrophils | ANC | |
|---|---|---|---|---|
| May 7 | 900 | 0.6 | 540 | |
| May 8 | 850 | 0.59 | 502 | |
| May 9 | 720 | 0.7 | 504 | |
| May 10 | 300 | 0.45 | 135 | |
| May 11 | 15 | No differential | — | |
| May 12 | 30 | No differential | — | |
| May 13 | 50 | No differential | — | |
| May 14 | 250 | 0.4 | 100 | |
| May 15 | 800 | 0.7 | 560 | Date of first recovery: ANC ≥ 0.5×109/L |
| May 16 | 1050 | 0.8 | 840 | |
| May 17 | 1000 | 0.7 | 700 | |
| May 18 | 1800 | 0.6 | 1080 | |
| May 19 | 2000 | 0.55 | 1100 | |
| May 20 | 2500 | 0.53 | 1325 | |
| May 21 | 2250 | 0.43 | 968 | |
| May 22 | 1500 | 0.45 | 675 |
Question 4: Was there evidence of initial hematopoietic recovery?
Indicate whether or not there was evidence of initial ANC recovery following this HCT.
Check only one response:
- If Yes if ANC ≥ 500/mm3 (or ≥ 0.5 × 109/L) achieved and sustained for 3 laboratory values.
- If No if ANC ≥ 500/mm3 (or ≥ 0.5 × 109/L) was not achieved.
- Check Not applicable if the recipient’s ANC never dropped below 0.5 × 109/L at any time post-HCT. This option is only applicable in the 100-day reporting period.
- Check Previously reported if this is the 6-month or annual follow-up, and the initial ANC recovery has already been reported.
Question 5: Date ANC ≥ 500/mm3 (first of 3 lab values)
Enter the first date of the three consecutive laboratory values obtained on different days where the ANC was ≥ 500/mm3 (or ≥ 0.5 × 109/L). For an example of tracking ANC recovery, see the Tracking ANC Recovery example above.
For more information regarding reporting partial or unknown dates, see General Instructions, General Guidelines for Completing Forms.
Question 6: Did late graft failure occur?
Late (or secondary) graft failure is defined when the recipient meets criteria for initial engraftment but subsequently develops loss of a previously functioning graft by development of at least two lines of cytopenia. Late graft failure is more often associated with allogeneic HCT than with autologous HCT. Some possible causes for late graft failure include graft rejection related to residual host immunity, persistent or progressive disease, low donor cell yield, medication side-effect, infection or GvHD.2
If the recipient meets the criteria of graft failure, check Yes.
2 Appelbaum, F. R., & Thomas, E. D. (2009). Thomas’ Hematopoietic Cell Transplantation: Stem Cell Transplantation (4th ed.). Chichester, UK: Wiley-Blackwell.
Section Updates:
| Question Number | Date of Change | Add/Remove/Modify | Description | Reasoning (If applicable) |
|---|---|---|---|---|
| . | . | . | . | . |
Need more help with this?
Don’t hesitate to contact us here.