The FormsNet3SM application allows questions 56-211 to be reported multiple times. Complete these questions for each line of therapy administered on or after the date of diagnosis of MPN and prior to the start of the preparative regimen (or prior to infusion if no preparative regimen was given). When submitting the paper version of the form for more than one line of therapy, copy the “Pre-HCT / Pre-Infusion Therapy” section and complete a copy of the section for each line of therapy administered.
A single line of therapy refers to any agents administered during the same time period with the same intent (induction, consolidation, etc.). If a recipient’s disease status changes resulting in a change to treatment, a new line of therapy should be reported. Additionally, if therapy is changed because a favorable disease response was not achieved, a new line of therapy should be reported.
Question 55: Was therapy given?
Indicate if the recipient received treatment for MPN after the time of diagnosis and before the start of the preparative regimen. If “yes,” continue with question 56. If “no,” continue with question 213.
Question 56: Date CBC with differential drawn
Report the date the sample was collected for testing and continue with question 57. If multiple studies were performed prior to the start of therapy, report the most recent lab immediately prior to this line of therapy.
Questions 57-58: WBC
Indicate whether the white blood cell (WBC) count was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the laboratory count and unit of measure documented on the laboratory report in question 58. If “unknown,” continue with question 59.
Questions 59-60: Neutrophils
Indicate whether the neutrophil percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the value documented on the laboratory report in question 60. If “unknown,” continue with question 61.
Questions 61-62: Bands
Indicate whether the band percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 62. If “unknown,” continue with question 63.
Questions 63-64: Metamyelocytes
Indicate whether the percentage of metamyelocytes in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 64. If “unknown,” continue with question 65.
Questions 65-66: Myelocytes
Indicate whether the myelocyte percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 66. If “unknown,” continue with question 67.
Questions 67-68: Lymphocytes
Indicate whether the lymphocyte percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 68. If “unknown,” continue with question 69.
Questions 69-70: Monocytes
Indicate whether the monocyte percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 70. If “unknown,” continue with question 71.
Questions 71-72: Basophil
Indicate whether the basophils percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 72. If “unknown,” continue with question 73.
Questions 73-74: Eosinophil
Indicate whether the eosinophil percentage in the blood was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 74. If “unknown,” continue with question 75.
Questions 75-76: Blasts in blood
Indicate whether the percent blasts in the peripheral blood is “known” or “unknown” prior to the start of this line of therapy. This may be determined by an automated differential, a manual count, or flow cytometry. If “known,” report the percentage documented on the laboratory report in question 76. Note, blasts are only reported on the differential if present. If there is no documentation of blasts, one can report 0%. If “unknown,” continue with question 77.
Questions 77-78: Hemoglobin
Indicate whether the hemoglobin was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the laboratory count and unit of measure documented on the laboratory report in question 77. If “unknown,” continue with question 80.
Question 79: Were RBC transfused ≤ 30 days before the date the CBC was drawn?
Transfusions temporarily increase the red blood cell count. It is important to distinguish between a recipient whose body is creating these cells and a recipient who received these cells from a transfusion.
Indicate if red blood cells were transfused less than or equal to 30 days prior to the date the CBC was drawn.
Questions 80-81: Platelets
Indicate whether the platelet count was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the laboratory count and unit of measure documented on the laboratory report in question 81. If “unknown,” continue with question 83.
Question 82: Were platelets transfused ≤ 7 days before the date the CBC was drawn?
Transfusions temporarily increase the platelet count. It is important to distinguish between a recipient whose body is creating the platelets and a recipient who received these cells from a transfusion.
Indicate if platelets were transfused less than or equal to 7 days prior to the date the CBC was drawn.
Questions 83-85: Blasts in bone marrow
Indicate whether the percentage of blasts in the bone marrow was “known” or “unknown” prior to the start of this line of therapy. If “known,” report the percentage documented on the laboratory report in question 84 and the date of sample collection in question 85. If “unknown,” continue with question 86.
Questions 86: Did the recipient have constitutional symptoms ( > 10% weight loss in six months, night sweats, unexplained fever higher than 37.5°C)?
Indicate if constitutional symptoms were present prior to the start of this line of therapy. Constitutional symptoms are often called “B” symptoms and include unexplained fever greater than 37.5°C (99.5°F), night sweats, or unexplained weight loss in the six months before the last evaluation prior to the start of this line of therapy.
Report “yes” if any constitutional symptoms were present prior to the start of this line of therapy.
Report “no” if constitutional symptoms were not present at this timepoint.
Report “unknown” if it is not possible to determine the presence or absence of constitutional symptoms at this timepoint.
Question 87-96: Were tests for driver mutations performed?
Testing for driver mutations may be performed by different methods including next generation sequencing (NGS), polymerase chain reaction (PCR), microarray, and fluorescence in situ hybridization (FISH). If testing was performed by any / all of these methods prior to the start of this line of therapy to assess JAK2, CALR, MPL and CSF3R, report “yes” for question 87 and continue with question 88.
If testing for driver mutations was not performed or is unknown, report “no” or “unknown” and continued with question 98.
Question 97: Was documentation submitted to the CIBMTR?
Indicate whether documentation was submitted to the CIBMTR (e.g., laboratory report, FISH report). For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide .
Question 98: Were tests for molecular markers performed (e.g., PCR)? (please do not include driver mutations JAK2, CALR, MPL, and CSF3R as previously captured above)
Molecular assessment involves testing blood or bone marrow for the presence of known molecular markers associated with the recipient’s disease. Molecular assessments are the most sensitive test for genetic abnormalities and involve amplifying regions of cellular DNA by polymerase chain reaction (PCR), typically using RNA to generate complementary DNA through reverse transcription (RT-PCR). The amplified DNA fragments are compared to a control, providing a method of quantifying log increase of genetic mutation transcripts. Each log increase is a 10-fold increase of gene transcript compared to control.
Indicate if molecular studies were obtained prior to the start of this line of therapy. If “yes” continue with question 99.
If no molecular studies were obtained or it is unknown if molecular studies were performed, select “no” or “unknown” and continue with question 163.
Question 99: Indicate if a positive molecular marker(s) was identified
Indicate if a positive molecular marker was identified prior to the start of this line of therapy.
If a positive molecular marker was identified, select “yes” and continue with question 100.
If there were no molecular markers identified, select “no” and continue with question 163.
Question 100: Specify the total number of positive molecular markers:
Specify the total number of positive molecular markers, then continue with question 101.
Question 101: Date sample collected:
Report the date the sample was collected for molecular testing. If multiple studies were performed, report the most recent lab immediately prior to this line of therapy.
Questions 102-161: Specify the positive molecular marker:
Specify each positive molecular marker. If a positive marker is detected, but not listed as an option select “Other molecular marker” and specify the positive molecular marker in the “specify other molecular marker” data field. Additionally, indicate if the amino acid change is “known” or “unknown” for the positive molecular marker reported. If known, report the amino acid change.
Question 162: Was documentation submitted to the CIBMTR?
Indicate whether documentation was submitted to the CIBMTR for each molecular marker reported in Q102-161. For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide.
Question 163: Were cytogenetics tested (karyotyping or FISH)?
Cytogenetic analysis is the study of chromosomes. Cytogenetic assessment involves testing blood or bone marrow for the presence of known chromosomal abnormalities that reflect the recipient’s disease. Testing methods include conventional chromosome analysis (karyotyping) or fluorescence in situ hybridization (FISH). For more information about cytogenetic testing and terminology, see Appendix C, Cytogenetic Assessments.
Karyotyping is performed by culturing cells (growing cells under controlled conditions) until they reach their dividing phase. Techniques are then performed to visualize the chromosomes during cell division so that various bands and reconfigurations can be seen. Banding pattern differentiation and chromosomal reconfiguration demonstrated evidence of disease.
FISH is a sensitive technique that assesses a large number of cells. This technique uses special probes that recognize and bind to fragments of DNA. These probes are mixed with cells from the recipient’s blood or bone marrow. A fluorescent “tag” is then used to visualize the binding of the probe to the diseased cells. Additionally, the FISH probe panel should reflect the recipient’s current disease; FISH may be used as surveillance for changes associated with post-therapy malignancy.
FISH testing for sex chromosomes after sex-mismatched allogeneic HCT should not be considered a disease assessment as the purpose is to determine donor chimerism. Additionally, the FISH probe panel should reflect the recipient’s current disease; FISH may be used as surveillance for changes associated with post-therapy malignancy.
If cytogenetic (karyotyping or FISH) studies were obtained prior to the start of this line of therapy, report “yes” and continue with question 164.
If no cytogenetic studies were obtained prior to the start of this line of therapy, indicate “no” and continue with question 182.
If it is not known whether any cytogenetic studies were obtained prior to the start of this line of therapy, indicate “unknown” and go to question 182.
Question 164: Were cytogenetics tested via FISH?
If FISH studies were performed prior to the start of this line of therapy, report “yes” and continue with question 165. If FISH studies were not performed prior to this line of therapy, report “no” and go to question 173. Examples include: no FISH study performed or FISH sample was inadequate. See Appendix C, Cytogenetic Assessments, for assistance interpreting FISH results.
Questions 165-166: Sample source:
Indicate if the sample was from “bone marrow” or from “peripheral blood” and report the date the sample was collected question 166. If multiple sources were used to test FISH, the most preferred sample is the bone marrow.
Question 167: Results of tests:
If FISH assessments identified abnormalities, indicate “abnormalities identified” and continue with question 168.
If FISH assessments were unremarkable, indicate “no abnormalities” identified, continue with question 172.
Question 168-171: Specify cytogenetic abnormalities (FISH)
Report the International System for Human Cytogenetic Nomenclature (ISCN) compatible string, if applicable, in question 168, then continue with question 169.
Report the number of abnormalities detected by FISH prior to this line of therapy in question 169. After indicating the number of abnormalities in question 169, select all abnormalities detected in questions 170-171.
If an abnormality is detected, but not listed as an option in question 170, select “other abnormality” and specify the abnormality in question 171. If multiple “other abnormalities” were detected, report “see attachment” in question 171 and attach the final report(s) for any other abnormalities detected. For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide .
Question 172: Was documentation submitted to the CIBMTR?
Indicate whether documentation was submitted to the CIBMTR (e.g., pathology report, FISH report). For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide .
Question 173: Were cytogenetics tested via karyotyping?
If karyotyping was performed prior to the start of this line of therapy report “yes” and continue with question 174.
If karyotyping was not performed at this time point, indicate “no” and continue with question 182. Examples of this include: karyotyping was not performed, or karyotyping sample was inadequate.
Questions 174-175: Sample source:
Indicate if the sample was from “bone marrow” or from “peripheral blood” and report the date the sample was collected question 175. If multiple sources were used for karyotyping analyses, the most preferred sample is the bone marrow.
Question 176: Results of tests:
If karyotyping assessments identified abnormalities, indicate “abnormalities identified” and continue with question 177.
If karyotyping assessments yielded no evaluable metaphases or there were no abnormalities identified, indicate such and continue with question 181.
Question 177-180: Specify cytogenetic abnormalities (karyotyping)
Report the International System for Human Cytogenetic Nomenclature (ISCN) compatible string, if applicable, in question 177, then continue with question 178.
Report the number of abnormalities detected by karyotyping prior to this line of therapy question 178. After indicating the number of abnormalities, select all abnormalities detected in questions 179-180.
If an abnormality is detected, but not listed as an option in question 179, select “other abnormality” and specify the abnormality in question 180. If multiple “other abnormalities” were detected, report “see attachment” in question 180 and attach the final report(s) for any other abnormalities detected. For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide.
Question 181: Was documentation submitted to the CIBMTR?
Indicate whether documentation was submitted to the CIBMTR (e.g., pathology report, karyotype report). For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide.
Question 182: Systemic Therapy
Systemic therapy refers to a delivery mechanism where a therapeutic agent is delivered orally or intravenously to the whole body. These drugs enter the bloodstream and are distributed throughout the body.
Indicate “yes” if the recipient received systemic therapy and continue with question 183. If the recipient did not receive systemic therapy, indicate “no” and continue with question 192.
Questions 183-184: Date therapy started:
Indicate whether the therapy start date is “known” or “unknown.” If the therapy start date is known, report the date the recipient first began this line of therapy in question 184. If the start date is partially known (e.g. the recipient started in mid-July 2010), use the process for reporting partial or unknown dates as described in the General Instructions, Guidelines for Completing Forms.
If the date therapy started is “unknown,” go to question 185.
Questions 185-186: Date therapy stopped:
Indicate if therapy stop date is “known” or “unknown.” If the therapy is being given in cycles, report the date the recipient started the last cycle for this line of therapy in question 186. If the therapy is administered in a single line or single administration, report the last day systemic therapy was administered. If the stop date is partially known, use the process for reporting partial or unknown dates as described in the General Instructions, Guidelines for Completing Forms.
If the date therapy stopped is “unknown,” go to question 187.
Questions 187-188: Specify reason therapy stopped:
Indicate the reason the line of therapy was stopped using one of the following options:
- Toxicity (e.g. cytopenia): The recipient developed a toxicity in response to therapy.
- Not tolerable: The recipient’s therapy was stopped due to intolerability (adverse events)
- Lack of response: The recipient’s course of treatment was stopped due to lack of a complete response.
- Disease progression: The recipient’s disease progressed from HI; Requires at least one of the following in the absence of another explanation (e.g., infection, bleeding, ongoing chemotherapy, etc.):
- ≥ 50% reduction from maximum response levels in granulocytes or platelets
- Reduction in hemoglobin by ≥ 1.5 g/dL
- Transfusion dependence
- Other: Use this option choice for any reason not included above and specify the reason in question 188.
- Unknown: Use this option when the reason therapy was stopped is unknown.
Questions 189-191: Specify systemic drugs given (check all drugs given as part of this line of therapy)
Treatments vary based on protocol. A treatment may consist of a single drug or a combination of drugs. Additionally, the drugs may be administered on one day, over consecutive days, or continuously. Select all chemotherapy drugs administered as part of this line of therapy.
If the recipient received a JAK1 or JAK2 inhibitor not listed, select “other JAK1 or JAK2 inhibitor” and report the agent in question 190.
If the recipient received a systemic therapy which is not listed, select “other systemic therapy” and report the agent in question 191. Report the generic name of the agent, not the name brand.
Question 192-193: Supportive treatment
Supportive treatment refers to therapy given to prevent, control, or relieve complications and side effects and to improve the recipient ‘s comfort. These therapies include treatment with growth factors (EPO, G-CSF, GM-CSF, etc.).
If the recipient received supportive treatment, report “yes” and select all supportive treatment given in question 193. If the recipient did not receive supportive treatment, report “no” and continue with question 194.
Question 194: Cellular Therapy (e.g. CAR-T cells)
Cellular therapy refers to the infusion of human derived cells, which may or may not be modified or processed to achieve a specific composition. Examples include T-cell, NK cell, and mesenchymal cell infusions as well as donor cellular infusions.
Report “yes” if the recipient received a cellular therapy as part of the line of therapy being reported. If not, report “no.”
Question 195-196: Blinded randomized trial
Indicate whether treatment was administered as part of a blinded randomized trial. Consult the physician overseeing treatment if it is not clear whether the therapy is being given as part of a blinded randomized trial. If “yes,” report the clinicaltrials.gov number in question 196. Otherwise, go to question 197.
If the clinical trial number (NCT number) is not clearly documented, it can be looked up using the Find a Study feature on www.clinicaltrials.gov.
If the recipient is participating in a clinical trial that is not registered with clinicaltrials.gov, but is registered elsewhere, leave question 196 blank and override the validation error using the code “Unable to answer.” Also, attach documentation which displays the clinical trial number and corresponding registry to the form in FormsNet3SM.
For further instructions on how to attach documents in FormsNet3SM, refer to the Training Guide.
Question 197: Splenic Radiation:
Report whether the recipient received splenic radiation and continue with question 198.
Question 198-199: Splenectomy:
Indicate if the recipient underwent a splenectomy. If the recipient had a splenectomy, report the splenectomy date in question 199. If the recipient did not have a splenectomy, continue with question 200.
Questions 200-201: Other therapy
Report whether the recipient received additional therapy which does not fit into the previous form categories. Examples may include intrathecal therapy or surgery. Specify the other therapy given in question 201.
Question 202: Best response to line of therapy:
Indicate the MPN disease response to each line of therapy using the definitions found in the text on FormsNet3SM. These definitions are also located in the MPN Response Criteria .
If the recipient’s disease status was “Complete remission (CR),” “Partial clinical remission (PR),” “Stable disease (SD),” “Progressive disease,” “Relapse,” or “Progression to AML (AML),” continue with question 206.
If the recipient’s disease status was “Clinical improvement (CI),” continue with question 203.
If the disease status was “not assessed,” continue with question 207.
Question 203: Was an anemia response achieved?
Specify if an anemia response has been achieved at the time of best response to this line of therapy and continue with question 204.
An anemia response is characterized by a ≥20 g/L increase in hemoglobin level (for transfusion-independent recipients) or by becoming transfusion-independent (transfusion-dependent recipients).
Question 204: Was a spleen response achieved?
Specify if a spleen response has been achieved at the time of best response to this line of therapy and continue with question 205.
A spleen response is achieved when a baseline splenomegaly that is palpable at 5-10 cm below the left costal margin (LCM) becomes not palpable or baseline splenomegaly that is palpable at >10 cm below the LCM, decreases by ≥50%.
A baseline splenomegaly that is palpable at <5 cm, below the LCM, is not eligible for spleen response.
A spleen response can be documented by a physician or confirmed by MRI / computed tomography showing ≥35% spleen volume reduction.
Question 205: Was a symptom response achieved?
The Myeloproliferative Neoplasm Symptom Assessment Form Total Symptom Score (MPN-SAF TSS) is used to evaluate the recipient’s symptom response. The MPN-SAF TSS is used to provide an accurate assessment of MPN symptom burden. The evaluation tool allows recipients with MPN to report their symptom severity at the worst level. They rate their symptom severity on a scale from zero to ten, zero being absent to ten being the worst imaginable. Adding the scores for all symptoms together will result in the recipient’s MPN-SAF TSS. See Table 3 below for an example of this assessment:
Table 3 . Myeloproliferative Neoplasm Symptom Assessment Form Total Symptom Score (MPN-SAF TSS)
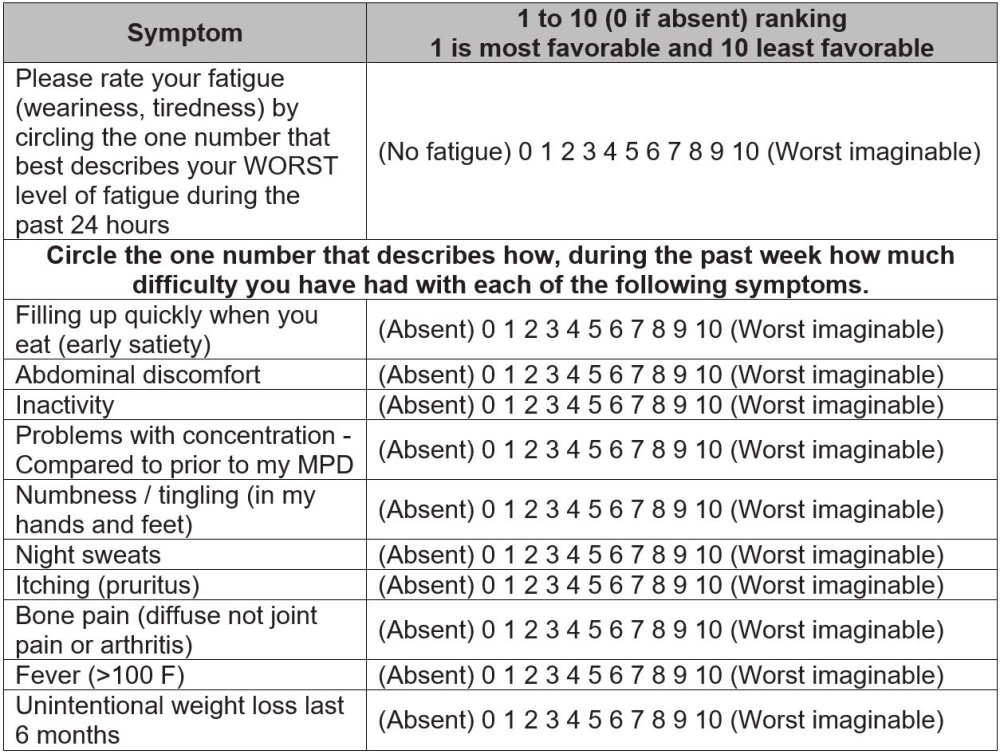
A symptom response is achieved when there is a ≥50% reduction in the Myeloproliferative Neoplasm Symptom Assessment Form Total Symptom Score (MPN-SAF TSS).
Specify if a symptom response has been achieved at the time of best response to this line of therapy and continue with question 206.
Question 206: Date assessed:
Enter the date the best response to the line of therapy was established. Report the date of the pathological evaluation (e.g., bone marrow biopsy), or the date of blood/serum assessment (e.g., CBC, peripheral blood smear) used to establish the best response to the line of therapy. Enter the date the sample was collected for pathological and/or laboratory evaluations. If the recipient was treated for extramedullary disease and a radiological assessment (e.g., X-ray, CT scan, MRI scan, PET scan) was performed to assess disease response, enter the date the imaging took place for radiologic assessments. If no pathological, radiographic, or laboratory assessment was performed to establish the best response to the line of therapy, report the office visit in which the physician clinically assessed the recipient’s response
If the exact date is not known, use the process for reporting partial or unknown dates as described in General Instructions, Guidelines for Completing Forms.
Question 207: Specify the cytogenetic response:
Specify the recipient’s cytogenetic response at the time of best response to this line of therapy.
If there is eradication of the previous reported abnormality select “Complete response (CR)” and continue with question 208.
If there is a ≥ 50% reduction in abnormal metaphases, select “Partial Remission (PR)” and continue with question 208.
Select “Re-emergence of pre-existing cytogenetic abnormality” if the cytogenetic abnormality was eradicated and reemerged at the time of best response to this line of therapy and continue with question 208.
If cytogenetic response was not tested at the time of best response to this line of therapy select “Not assessed” and continue with question 209.
Select “not applicable” if cytogenetic abnormalities were never identified and continue with question 209.
If the recipient does not meet the criteria for CR or PR, select “None of the above” and continue with question 208 (e.g. if a new cytogenetic abnormality is identified but there is also eradication of a previous abnormality).
Example: A recipient had 10 abnormal metaphases (out of 20) at diagnosis. At the time of their best response to this line of therapy, they had 2 abnormal metaphases (out of 20). As this is a ≥50% reduction in abnormal metaphases, “Partial Remission (PR)” should be reported.
Question 208: Date assessed:
Report the date the cytogenetic response was established. Enter the date the sample was collected for pathologic evaluation (e.g., bone marrow biopsy) or blood / serum assessment.
Question 209: Specify the molecular response:
Specify the recipient’s molecular response at the time of best response to this line of therapy evaluation.
If there is eradication of the previous reported abnormality, select “Complete response (CR)” and continue with question 210.
If there is a 50% decrease in allele burden, select “Partial Remission (PR)” and continue with question 210.
Select “Re-emergence of pre-existing molecular abnormality” if the molecular abnormality was eradicated and reemerged at the time of best response to this line of therapy and continue with question 210.
If molecular response was not tested at the last evaluation select “Not assessed” and go to question 211.
Select “not applicable” if molecular abnormalities were never identified and go to question 211.
If the recipient does not meet the criteria for CR or PR, select “None of the above” and continue with question 210 (e.g. if a new molecular abnormality is identified but there is also eradication of a previous abnormality).
Example: A recipient had an allele burden of 50% at diagnosis. At the time of their best response to this line of therapy, they had an allele burden of 25%. As this is a ≥50% reduction in the allele burden, “Partial Remission (PR)” should be reported.
Question 210: Date assessed:
Report the date the molecular response was established. Enter the date the sample was collected for pathologic evaluation (e.g., bone marrow biopsy) or blood/serum assessment.
Question 211: Did disease relapse / progress following this line of therapy?
Refer to the MPN Response Criteria section when determining the recipient’s disease status. Indicate if the disease relapsed from CR or progressed. Report ‘Yes” if the relapse or progression criteria was met after starting this line of therapy and prior to starting the subsequent line of therapy.
Question 212: Date of relapse/progression:
Enter the date of the assessment that established relapse or progression after starting this line of therapy. Enter the date the sample was collected for pathological and laboratory evaluations. If extramedullary disease is detected upon radiographic examination (e.g., X-ray, CT scan, MRI scan, PET scan), enter the date the imaging took place. If the physician determines cytogenetic or molecular relapse, enter the date of sample collection for cytogenetic or molecular evaluation. If the physician determines evidence of relapse following a clinical examination during an office visit, report the date of assessment.
If the exact date is not known, use the process for reporting partial or unknown dates as described in General Instructions, Guidelines for Completing Forms.
Copy questions 56 – 212 if needed for multiple lines of therapy.
Section Updates:
| Question Number | Date of Change | Add/Remove/Modify | Description | Reasoning (If applicable) |
|---|---|---|---|---|
| Q194 | 6/28/2023 | Add | The Reporting Prior Cellular Therapy as a Line of Therapy blue information box added: As of June 28, 2023, the ‘cellular therapy’ option within the Pre-Infusion Lines of Therapy section is no longer enabled. Recipients who received a cellular therapy prior to the current infusion is no longer required to be reported as a line of therapy on the pre-infusion disease specific form | Due to change in FormsNet3 validation |
| Q206 | 5/6/2022 | Modify | Clarified instructions on how to report the best response to therapy assessment date: |
Previous instructions were for how to report the pre-infusion disease status assessment date. Updated to reflect instructions for reporting the best response to line of therapy assessment date. |
| Q211 | 7/25/2025 | Modify | Clarified how to report relapse / progression: Refer to the MPN Response Criteria section when determining the recipient’s disease status. Indicate if the disease relapsed from CR or progressed. |
Added for clarification |
| Q212 | 7/25/2025 | Modify | Clarified how to report the relapse / progression date: Enter the date of the assessment that established relapse or progression |
Added for clarification |
Need more help with this?
Don’t hesitate to contact us here.

