Need more help with this?
Don’t hesitate to contact us here.



- Getting Started
- General Instructions
- Recipient Assignment, Indication, and Information Manuals
- Transplant Essential Data (TED) Manuals
- 2400: Pre-TED
- Q1 – 21: Recipient Information
- Q22 – 41: Hematopoietic Cellular Transplant (HCT) and Cellular Therapy
- Q42 – 80: Donor Information
- Q81 – 86: Clinical Status of Recipient Prior to the Preparative Regimen (Conditioning)
- Q87 – 119: Comorbid Conditions
- Q120 – 134: Pre-HCT Preparative Regimen (Conditioning)
- Q135 – 139: Additional Drugs Given in the Peri-Transplant Period
- Q140 – 142: GVHD Prophylaxis
- Q143 – 145: Planned Post-HCT Disease Therapy Planned as of Day 0
- Q146: Prior Exposure: Potential Study Eligibility
- Q147 – 157: COVID-19 (SARS-CoV-2) Impact on Hematopoietic Cell Transplantation (HCT)
- 2402: Disease Classification
- Q1-2: Primary Disease for HCT / Cellular Therapy
- Q3 – 103: Acute Myelogenous Leukemia
- Q104 – 180: Acute Lymphoblastic Leukemia
- Q180 – 183: Acute Leukemias of Ambiguous Lineage and Other Myeloid Neoplasms
- Q184 – 194: Chronic Myelogenous Leukemia
- Q195 – 272: Myelodysplastic Diseases
- Q273 – 385: Myeloproliferative Diseases
- Q386 – 392: Other Leukemia
- Q393 – 410: Hodgkin and Non-Hodgkin Lymphoma
- Q411 – 457: Multiple Myeloma / Plasma Cell Disorder
- Q458 – 459: Solid Tumors
- Q460 – 462: Severe Aplastic Anemia
- Q463: Inherited Bone Marrow Failure Syndromes
- Q464 – 499: Hemoglobinopathies
- Q500 – 507: Disorders of Immune System
- Q508 – 509: Inherited Abnormalities of Platelets
- Q510 – 512: Inherited Disorders of Metabolism
- Q513 – 517: Histiocytic Disorders
- Q518 – 521: Autoimmune Diseases
- Q522 – 523: Tolerance Induction Associated with Solid Organ Transplant
- Q524: Other Disease
- 2450: Post-TED
- Q1 – 2: Survival
- Q3: Subsequent Infusion
- Q4 – 6: Initial ANC Recovery
- Q7 – 8: Initial Platelet Recovery
- Q9 – 34: Graft versus Host Disease (Allogeneic Only)
- Q35 – 37: Liver Toxicity Prophylaxis
- Q38 – 39: Veno-occlusive disease (VOD) / Sinusoidal obstruction syndrome (SOS)
- Q40 – 46: Infection
- Q47: New Malignancy, Lymphoproliferative or Myeloproliferative Disorder
- Q48 – 65: Chimerism Studies (Cord Blood Units, Beta Thalassemia, and Sickle Cell Disease Only)
- Q66- 88: Disease Assessment at the Time of Best Response to Infusion
- Q89 – 97: Post-Infusion Therapy
- Q98 – 108: Relapse or Progression Post-Infusion
- Q109 – 111: Current Disease Status
- 2400: Pre-TED
- Comprehensive Baseline & Follow-up Manuals
- 2000: Recipient Baseline
- Q1-3:Clinical Status of Recipient Prior to the Preparative Regimen (Conditioning)
- Q4-22: Organ Function Prior to the Preparative Regimen (Conditioning)
- Q23-34: Hematologic Findings Prior to the Preparative Regimen (Conditioning)
- Q35-38: Infection
- Q39-85: Pre-HCT Preparative Regimen (Conditioning)
- Q86-103: Additional Drugs Given in the Peri-Transplant Period
- Q104-117: Socioeconomic Information
- 2004: Infectious Disease Markers
- 2005: Confirmation of HLA Typing
- 2006: Hematopoietic Stem Cell Transplant (HCT) Infusion
- 2100: Post-Infusion Follow-Up
- Q1 – 9: Vital Status
- Q10 – 16: Granulopoiesis / Neutrophil Recovery
- Q17 – 20: Megakaryopoiesis / Platelet Recovery
- Q21 – 29: Growth Factor and Cytokine Therapy
- Q30 – 39: Current Hematologic Findings
- Q40 – 55: Immune Reconstitution
- Q56: Gene Therapy Persistence Testing
- Q57 – 74: Chimerism Studies
- Q75 – 85: Engraftment Syndrome
- Q86 – 134: Acute Graft vs. Host Disease (GVHD)
- Q135 – 204: Chronic Graft vs. Host Disease (GVHD)
- Q205 – 211: Current GVHD Status
- Q212 – 227: Infection Prophylaxis
- Q228 – 249: Infection
- Q250 – 382: Organ Function
- Q383: New Malignancy, Lymphoproliferative or Myeloproliferative Disease / Disorder
- Q384 – 408: Functional Status
- 409 – 412: Subsequent HCT
- 2451: Chimerism Essential Data
- 2000: Recipient Baseline
- Comprehensive Disease-Specific Manuals
- 2010/2110: Acute Myelogenous Leukemia (AML)
- 2011/2111: Acute Lymphoblastic Leukemia (ALL)
- 2012/2112: Chronic Myeloid Leukemia (CML)
- CML Response Criteria
- 2012: CML Pre-Infusion Data
- Q1-17: Disease Assessment at Diagnosis
- Q18-83: Laboratory Studies at Diagnosis
- Q84-185: Pre-HCT or Pre-Infusion Therapy
- Q186-191: Disease Assessment at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q192-252: Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q253-256: Disease Status at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- 2112: CML Post-Infusion Data
- 2013/2113: Chronic Lymphocytic Leukemia (CLL)
- 2014/2114: Myelodysplastic Syndrome (MDS)
- MDS Response Criteria
- 2014: Myelodysplastic Syndrome (MDS) Pre-Infusion
- Q1: Subsequent Transplant of Cellular Therapy
- Q2-17: Disease Assessment at Diagnosis
- Q18-47: Diagnostic Studies (Measured Prior to First Disease Treatment)
- Q48-81: IPSS-R Prognosis Score
- Q82-156: Pre-HCT / Pre-Infusion Therapy
- Q157-193: Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q194-208: Disease Assessment at Last Evaluation Prior to the Start of the Preparative Regimen
- 2114: Myelodysplastic Syndrome (MDS) Post-Infusion
- 2015/2115: Juvenile Myelomonocytic Leukemia (JMML)
- JMML Response Criteria
- 2015: JMML Pre-HCT
- Q1-6: Clinical Features at Diagnosis
- Q7-48: Laboratory Values at Diagnosis
- Q49-62: Pre-HCT Therapy
- Q63-64: Transformation
- Q65-91: Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen
- Q92-93: Disease Status at Last Evaluation Prior to the Start of the Preparative Regimen
- 2115: JMML Post HCT
- 2016/2116: Plasma Cell Disorders (PCD)
- Multiple Myeloma Response Criteria
- Plasma Cell Leukemia Response Criteria
- POEMS Response Criteria
- Amyloidosis Response Criteria
- 2016: PCD Pre-Infusion
- Q1-2: Disease Assessment at Diagnosis
- Q3-60: Diagnostic Studies (Measured Prior to Any Disease Treatment)
- Q61-124: Amyloidosis Organ Involvement at Diagnosis
- Q125-156: POEMS Syndrome Assessment at Diagnosis
- Q157-187: Pre-Infusion Therapy
- Q188-254:Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q255-289: Amyloidosis Organ Involvement at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q290-295: POEMS Syndrome Assessment at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- 2116: PCD Post-Infusion
- Q1-2: Disease Specificity
- Q3-53: Disease Assessment at the Time of Best Response to HCT or Cellular Therapy
- Q54-109: Organ Parameters of Amyloidosis at the Time of Best Response
- Q110-141: POEMS Syndrome Assessment at the Time of Best Response
- Q142-210: Post-Infusion Therapy
- Q211-252: Disease Status at the Time of Evaluation for this Reporting Period
- Q253-311: Current Status of Amyloidosis for this Reporting Period
- Q312 – 343: Current Status of POEMS Syndrome for This Reporting Period
- 2018/2118: Hodgkin and Non-Hodgkin Lymphoma
- Lymphoma Response Criteria
- 2018: LYM Pre-Infusion
- Q1-55: Disease Assessment at Diagnosis
- Q56-68: Laboratory Studies at Diagnosis
- Q69-81: Assessment of Nodal and Organ Involvement at Diagnosis
- Q82-139: Disease Assessment at Transformation
- Q140-152: Laboratory Studies at Transformation
- Q153-165: Assessment of Nodal and Organ Involvement at Transformation
- Q166-223: Pre-HCT Therapy
- Q224-233: Disease Assessment at the Failure of the 1st Line of Therapy (DLBCL only)
- Q234-288: Disease Assessment at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- 2118: LYM Post-Infusion
- 2019/2119: Waldenström’s Macroglobulinemia (WM)
- Waldenstrom’s Macroglobulinemia Response Criteria
- 2019: WM Pre-HCT
- Q1-2: Disease Assessment at Diagnosis
- Q3-23: Clinical Features Present at Diagnosis
- Q24-75: Laboratory Studies at Diagnosis
- Q76-120: Pre-HCT Therapy
- Q121-150: Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen
- Q151-152: Disease Status at Last Evaluation Prior to the Preparative Regimen
- 2119: WM Post-HCT
- 2026/2126: Neuroblastoma
- 2028/2128: Aplastic Anemia
- 2029/2129: Fanconi Anemia / Constitutional Anemia
- 2030/2130: Sickle Cell Disease (SCD)
- 2030: SCD Pre-Infusion
- Q1: Subsequent Infusion
- Q2 – 5: Sickle Cell Diagnosis
- Q6 – 16: Transfusion Therapy
- Q17 – 19: Therapy for Iron Overload
- Q20 – 24: Pulmonary Assessments
- Q25 – 34: Cardiovascular Assessments
- Q35 – 40: Renal Assessments
- Q41 – 45: Splenic Assessments
- Q46 – 50: Acute Chest Syndrome
- Q51 – 53: Pain
- Q54 – 56: Avascular Necrosis
- Q57 – 65: Central Nervous System
- Q66 – 76: Other Symptoms
- Q77 – 87: Existing Organ Impairments
- Q88 – 94: Disease Modifying Therapies
- Q95 – 118: Other Laboratory Studies
- Q119 – 120: Reason for Infusion
- Q121: Marrow Evaluation at Last Evaluation
- 2130: SCD Post-Infusion
- Q1 – 5: Physical Assessments
- Q6 – 8: Transfusion Therapy
- Q9 – 22: Therapy for Iron Overload
- Q23 – 27: Pulmonary Assessments
- Q28 – 48: Cardiovascular Assessments
- Q49 – 58: Hepatic Assessments
- Q59 – 65: Renal Assessments
- Q66 – 70: Splenic Assessments
- Q71 – 74: Acute Chest Syndrome
- Q75 – 80: Pain
- Q81 – 83: Avascular Necrosis
- Q84 – 92: Central Nervous System
- Q93 – 104: Other Symptoms
- Q105 – 116: Existing Organ Impairments
- Q117 – 123: Disease Modifying Therapies
- Q124 – 147: Other Laboratory Studies
- Q148: Disease Status
- Q149: Marrow Evaluation
- 2030: SCD Pre-Infusion
- 2031/2131: Immune Deficiencies (ID)
- 2033/2133: Wiskott-Aldrich Syndome (WAS)
- 2034/2134: X-Linked Lymphoproliferative Sydrome (XLP)
- 2034: XLP Pre-HCT
- Q1-23: Disease Assessment at Diagnosis
- Q24-32: History of Epstein Barr Virus (EBV) Infection
- Q33-51: Assessment of Immunologic Function at Diagnosis
- Q52-104: Disease Assessment between Diagnosis and the Start of the Preparative Regimen
- Q105-130: Disease Status at Last Evaluation Prior to the Start of the Preparative Regimen
- 2134: XLP Post-HCT
- 2034: XLP Pre-HCT
- 2037 / 2137 Leukodystrophies
- 2039/2139: Hemophagocytic Lymphohistiocytosis (HLH)
- 2039: HLH Pre-HCT
- Q1-22: Disease Assessment at Diagnosis
- Q23-47: Clinical Features and Laboratory Studies at Diagnosis
- Q48-58: Disease Assessment Between Diagnosis and the Start of the Preparative Regimen
- Q59-74: History of Infection at Any Time Prior to the Preparative Regimen
- Q75-107: Pre-HCT Therapy
- Q108-127: Clinical Features and Laboratory Studies At Last Evaluation Prior to the Start of the Preparative Regimen
- 2139: HLH Post-HCT
- 2039: HLH Pre-HCT
- 2057/2157 Myeloproliferative Neoplasms (MPN)
- MPN Response Criteria
- 2057: Myeloproliferative Neoplasm (MPN) Pre-Infusion
- Q1: Subsequent Transplant
- Q2-10: Disease Assessment at Diagnosis
- Q11-40: Diagnostic Studies (Measured Prior to First Disease Treatment)
- Q41-54: DIPSS Prognosis Score
- Q55-212: Pre-HCT / Pre-Infusion Therapy
- Q213-254: Laboratory Studies at Last Evaluation Prior to the Start of the Preparative Regimen / Infusion
- Q255-261: Disease Assessment at the Last Evaluation Prior to the Preparative Regimen / Infusion
- 2157: Myeloproliferative Neoplasm (MPN) Post-Infusion
- 2058/2158: Thalassemia
- 2058: Thalassemia Pre-Infusion
- Q1: Subsequent Transplant or Cellular Therapy
- Q2 – 26: Thalassemia Diagnosis
- Q27 – 52: Donor Related Information
- Q53 – 59: Transfusion Therapy
- Q60 – 62: Hepatic Assessments
- Q63 – 72: Cardiac Assessments
- Q73 – 75: Renal Assessments
- Q76– 78: Avascular Necrosis
- Q79: Other Symptoms
- Q80 – 89: Additional Iron Overload Assessments
- Q90 – 94: Additional Hematologic Labs
- Q95 – 105: Specify Existing Organ Impairments
- Q106 – 112: Disease Modifying Therapy
- Q113: Marrow Evaluation
- 2158: Thalassemia Post-Infusion
- Q1 – 15: Post-Infusion Disease Testing
- Q16 – 17: Transfusion Therapy
- Q18 – 29: Treatment
- Q30 – 31: Splenic Assessments
- Q32 – 55: Hepatic Assessments
- Q56 – 68: Cardiac Assessments
- Q69 – 73: Renal Assessments
- Q74 – 76: Avascular Necrosis
- Q77: Other Symptoms
- Q78 – 92: Additional Iron Overload Assessments
- Q93 – 101: Additional Hematologic Labs
- Q102 – 113: Specify Existing Organ Impairments
- Q114 – 121: Disease Modifying Therapies
- Q122: Marrow Evaluation
- 2058: Thalassemia Pre-Infusion
- 2059/3507: Solid Tumor
- RECIST criteria
- 2059: Solid Tumor Pre-Infusion
- Q1: Subsequent Infusion
- Q2-26: Disease Assessment at Diagnosis
- Q27-31: Initial Therapy
- Q32-42: Last Line of Therapy Prior to Collection
- Q43-52: Bridging Therapy Prior to Infusion
- Q53-77: Total Cumulative Exposure to Systemic Therapy / Radiation Therapy
- Q78-102: Disease Assessments at Last Evaluation
- 3507: Solid Tumor Response
- Cellular Therapy Manuals
- 4000: Cellular Therapy Essential Data Pre-Infusion
- Q1-17: Recipient Data
- Q18-32: Cellular Therapy and HCT History
- Q33-52: Product Identification
- Q53-72: Indication for Cellular Therapy
- Q73: Lymphodepleting Therapy Prior to Cellular Therapy
- Q74-76: Hematologic Findings Prior to Lymphodepleting Therapy
- Q77-80: Functional Status
- Q81-91: Comorbid Conditions
- 4001: Pre-Cellular Therapy Baseline Data
- 4003: Cellular Therapy Product
- 4006: Cellular Therapy Infusion
- 4100: Cellular Therapy Essential Data Follow-Up
- Q1: Product
- Q2-3: Survival
- Q4-11: Subsequent Cellular Infusions
- Q12-14: Best Response to Cellular Therapy
- Q15-23: Peripheral Blood Count Recovery
- Q24-25: Disease Relapse or Progression
- Q26: New Malignancy, Lymphoproliferative or Myeloproliferative Disease / Disorder
- Q27-46: Graft vs. Host Disease
- Q47-177: Toxicities
- Q178-189: Infection
- Q190-191: Pregnancy Status
- 4101: Post-Cellular Therapy Follow-Up
- 4000: Cellular Therapy Essential Data Pre-Infusion
- Gene Therapy Manuals
- Infection & Miscellaneous Manuals
- 2046 / 2146: Fungal Infection
- 2047 / 2147: Hepatitis Serology
- 2149: Respiratory Virus Post-Infusion Data
- 2150: Viral Infection Diagnosis and Treatment Form
- 2199 Donor Lymphocyte Infusion
- 2553: VOD/SOS
- 2900: Recipient Death
- 3500: Subsequent Neoplasms
- 3501: Pregnancy Form
- 3502: Laboratory Studies
- 3503: Neurocognitive Assessment
- 3505: Transfusions
- 3506: Marrow Surveillance
- Study-Specific Manuals
- 2540: Tepadina® Supplemental Data
- 2541: Inotuzumab Ozogamacin (Besponsa™) Supplemental Data
- 2542: Mogamulizumab Supplemental Data Collection
- 2543: Mylotarg™ Supplemental Data Collection
- 2554: CMS Registration
- 2555: MF Eligibility
- 2565: Sanofi Mozobil Supplemental Data
- 2544: Betibeglogene Autotemcel (Zynteglo®) Pre-Infusion Supplemental Data
- 2545: Betibeglogene Autotemcel (Zynteglo®) Post-Infusion Supplemental Data
- 2546: Elivaldogene Autotemcel (Skysona®) Pre-Infusion Supplemental Data
- 2547: Elivaldogene Autotemcel (Skysona®) Post-Infusion Supplemental Data
- Appendices
- Appendix A: Abbreviations and Definitions
- Appendix B: Glossary of Terms
- Appendix C: Cytogenetics
- Appendix D: How to Distinguish Infusion Types
- Appendix E: Definition of a Product
- Appendix F: Response Evaluation Criteria in Solid Tumors (RECIST)
- Appendix G: Tracking Disease Status for Multiple Myeloma
- Appendix I: Ethnicity and Race
- Appendix J: Reporting Comorbidities
- Appendix L: Karnofsky / Lansky Performance Status
- Appendix N: Drug Classification
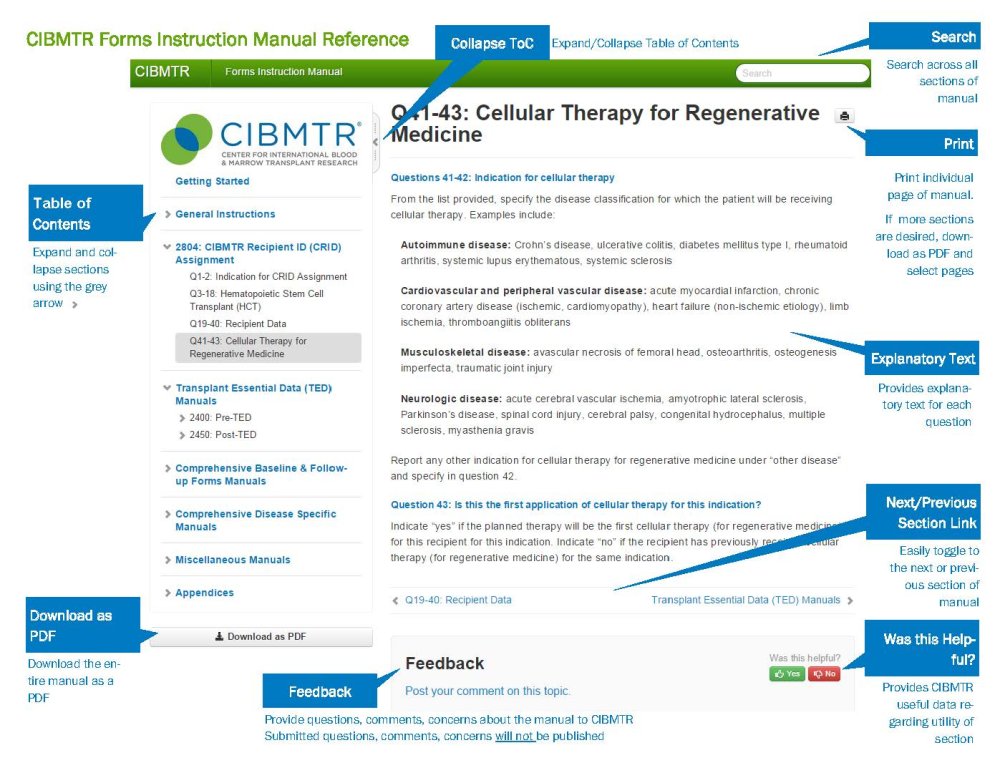
- Reporting Instruction Overview