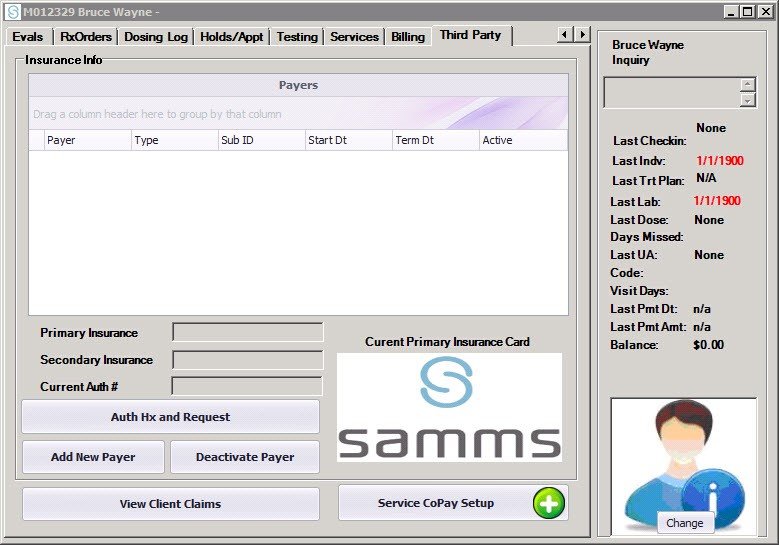
If an enrolling client has proof of third party health coverage, click on the Third Party tab in the client file.
- Click on Add New Payer
The Payer Enrollment screen will appear.
- Enter the Payer from the list of regional payers in the drop down menu.
- Select the Payer Type from the drop down as either primary or secondary.
- Enter the Subscriber ID (sometimes referred to as the Member ID), Group #, and Effective Date from the coverage ID card.
- Click Save to save the client’s payer information.
- Coverage details, including deductibles and co-pays will be added after the client is admitted to the program.
- Insurance ID cards may be scanned by clicking on the Scan Card button.
- The next step in this process is to verify third party eligibility. Please proceed to Checking Third Party Payer Eligibility.



Post your comment on this topic.