- To view the list, click on Third Party from the SAMMS main menu and select Billing Queue
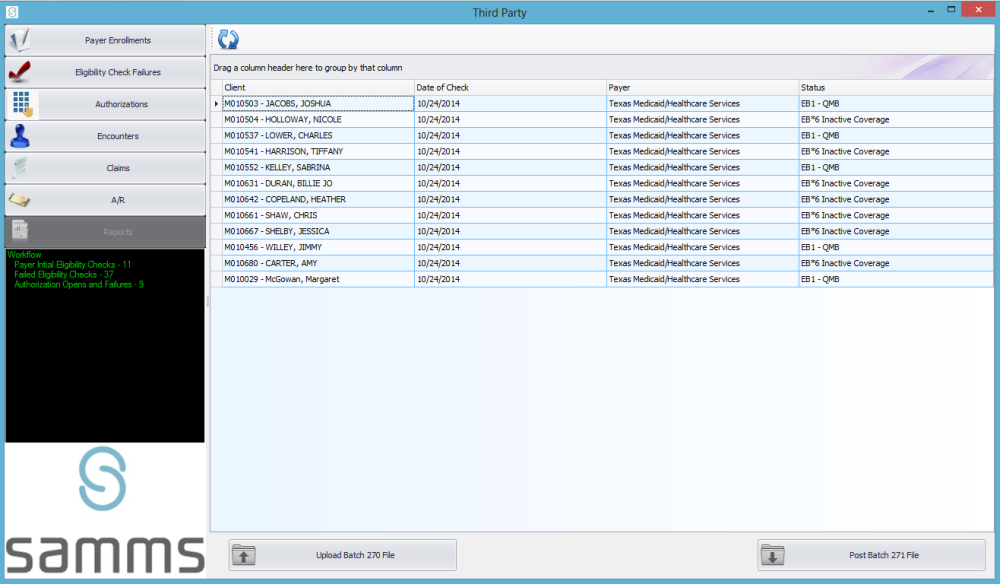
- Click on Eligibility Check Failures and a grid will display with the names and third party payer information for all clients showing as inactive.
- Click on the first client to be checked in the grid.
- The Manual Eligibility Check screen will display.
- Click on View Payer Info to view contact information for the third party payer.
- The Third Party Payer screen will display.
- Using the displayed Telephone number, contact the payer to confirm status.
- In the Manual Eligibility Check screen, select the Method you used to contact the third party payer from the drop down menu.
- From the drop down menu, select a Staff Decision on the disposition of the case.
- You may enter any additional information in the Staff Comment box.
By clicking on Post Response to Client Account, the new information is saved, and the client is removed from the Eligibility Check Failures list on the grid.



Post your comment on this topic.