Please note you should only be posting payments manually if you are not receiving Electronic Remittance Advice’s through the clearinghouse during your test billing phase or for isolated occurrences. Payments should be either posted automatically or via the payment report
Select Client/Employee/Doctor > “Billing” > Select a Transaction > “Submission Report.”
The Submission report has several different filter criteria you may use to pull the claims you’d like to post a payment to.
You can search by:
- Client
- Billing Status
- Start Date and End Date
- Search by Item ID
Once the search criteria have been chosen, click “Update View” to pull up the claims that fit the criteria you have entered.
Chose the claim you would like to apply payment to by clicking on the title.
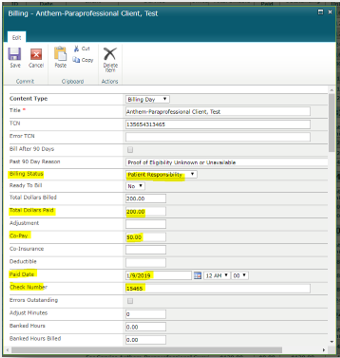
This will open a new window where you will enter the payment information that needs to be posted.
Click on “Edit Item”
From here, you can enter the Claim Number (TCN), Total Dollars Paid, Co-Pay, Co-Insurance, Deductible and any Adjustment amounts for this claim. You can also change the Billing Status to Received (claim paid in full), Patient Responsibility (co-pay, co-ins, deductible), etc. As well as the Paid Date and Check #.

If the claim has a Patient Responsibility, you will enter either the Co-Pay, Co-Insurance or Deductible amount in the corresponding field and change the billing status to Patient Responsibility. If the client has paid their Co-Pay, Co-Insurance or Deductible you will add that amount to the total dollars paid field, however you will not remove the Co-Pay, Co-Insurance or Deductible amount from that field.
For Example: This claim had a total billed amount of $200.00, the payor paid $150.00 with a Co-pay of $50.00. Your client has already paid you the $50.00 co-pay, so you will enter the “Total Dollars Paid” as $200.00 ($150 + $50 copay= $200 total dollars paid) and the Co-pay Amount as $50.00.
Once you have entered all the payment information for this claim you will click “Save”.









Post your comment on this topic.